Diabetic Foot
What is 'diabetic foot
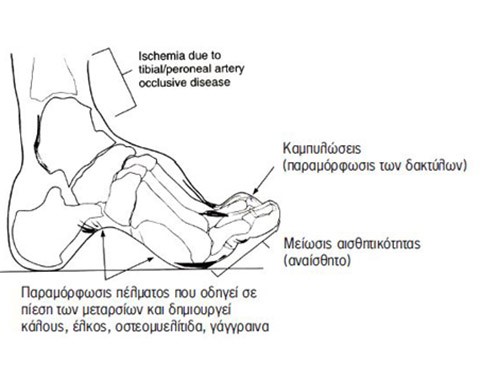
The term diabetic foot refers to changes in the foot that occur from the ankle to the toes. In reality, the sole turns downward and the toes bend upward.
How is the examination performed?
The examination lasts approximately 40-45 minutes. During the examination, the patient lies on their back on the MRI table and remains in continuous visual and auditory communication with the MRI technologist for anything needed.
At times, the patient may be asked to hold their breath for a few seconds following clear instructions from the technologist, to optimize the quality of the heart images produced. If the use of contrast material is required, a nurse will insert an intravenous catheter to administer the contrast medium, approximately halfway through the examination. After the examination, there are no restrictions; the patient can eat or drink freely and there is no need to avoid contact with children as no radioactive substances have been administered.
What are the causes of 'diabetic foot'?
Diabetes mellitus is a disorder of the metabolism of sugar, fat, and proteins. It affects every organ, but the main manifestations are summarized in a characteristic “triad.”
Neuropathy
Angiopathy
Reduced resistance to infections
Neuropathy
It affects the sensory and motor nerves, causing a polyneuropathy, specifically:
- The patient loses the sense of pain (note: pain warns us that something is wrong, and diabetics do not have this sensation).
- The patient loses the sense of pressure (they cannot feel if they are stepping on their shoe or a small stone).
- The patient loses the sense of foot position (they do not realize if they are stepping correctly or at an angle).
- The foot does not sweat (it becomes dry, and the skin easily cracks).
- Hair loss: sensitivity is lost (hairs act as antennas, signaling sensitivity).
- Muscle atrophy in the foot: The foot, from the ankle downward, has 42 muscles responsible for movement.
- A burning sensation, especially in the feet at night (the feet feel like they are burning).
What are the consequences of diabetic neuropathy?
All of the above, along with joint deformities (neuropathic arthropathy), lead to muscle weakness, significant foot deformity, the development of ulcers (neuropathic ulcers) which are overlooked due to the lack of pain and lead to bone infection (osteomyelitis), and ultimately, amputation.
Angiopathy (Narrowing of the blood vessels)
The blood vessels in diabetics are affected 15 times more often than in healthy individuals and are 10-15 years older than their actual age. Every blood vessel becomes obstructed, and depending on the organ affected, we observe the corresponding consequences.
What does diabetic angiopathy cause in the feet?
In the feet, the arteries below the knee are primarily obstructed. However, the main damage involves the mechanism of tissue nourishment from the blood vessels, as the vessel walls thicken, making it difficult for nutrients to pass through. Thus, we see normal blood vessels in diabetics, yet gangrene may occur due to a neglected injury.
What are the consequences of diabetic angiopathy?
- The patient is unable to walk (they experience cramping in the calf only when walking, they limp intermittently, and only when attempting to walk).
- The color of the foot changes, becoming pale or very red with swollen veins.
- The nails thicken or change shape.
Sensitivity to Infections
The body’s defense is significantly reduced, resulting in frequent infections caused by multiple bacteria simultaneously (polymicrobial infection).
How can we prevent an infection in the feet?
- Daily foot care with specific instructions.
- A “mirror” on the floor to observe the soles, heels, and toes daily.
What does the clinic offer for "diabetic foot"?
With the necessary initial preventive examinations and a clinical examination by a specialized vascular surgeon, the patient is included in the “Study Protocol” and regularly monitored. The initial tests include a blood test for specific markers, triplex ultrasound of the vessels, and X-rays of the foot extremities. Depending on any findings, the necessary treatment is provided to the patient and they are electronically monitored by the physician. It should be noted that all tests can be performed with an EOPYY referral and conducted within the clinic.
The “Diabetic Foot” Clinic was created in collaboration with the specialized vascular surgeon Dr. Georgios S. Koustas, MD PhD, Associate Professor, with primary training at Harvard University and further training at universities in France, Germany, and Brazil. He is a member of more than 8 international medical scientific societies, the Athens Medical Association, and the postgraduate programs at Harvard University. Dr. Koustas established and developed the first “Diabetic Foot” Clinics in Greece and has as his main collaborator Mrs. Athena Stoupi, Pathologist – Infectious Disease Specialist, Clinical Instructor at Warren Alpert Medical School of Brown University, USA.




